
Is There a Different Approach to Health Care?
Have you ever asked yourself this question?
How much do you truly understand about your health concerns—and the options available to you for care? I’ve been asking myself these questions more and more lately.
Though I work in healthcare, I’m not a medical professional. But I observe and experience the system every day, both at work and in my personal life. Recently, I’ve found myself wondering if there’s a different approach to pain management—something beyond appointments with little result, medications that offer no cure, and therapy that feels stagnant.
Please don’t get me wrong. I have deep respect for the physicians, surgeons, and medical staff I work alongside. But I also can’t shake the feeling that there must be something more—somewhere within or beyond the medical community—that can help people like me who have been in pain for far too long.
This curiosity led me down a new path, one that traditional practitioners don’t often talk about: mind-body connectionand the role our brain plays in chronic pain. I started researching on my own—Googling, watching YouTube videos, and listening to those who take a holistic approach. I’ve come to jokingly refer to myself as “Dr. Koshi” because of how deep I’ve gone in search of understanding.
One provider in particular caught my attention—someone who used to work in the very clinic where I’m employed. He left to pursue a different kind of care and has since authored three books on the mind-body relationship and pain. I’ve started reading one, and it’s opening my eyes to the idea that the brain can hold on to pain long after the body has healed.
I’ve brought this up with a few staff members, and I’ll admit, the conversation felt… uncomfortable. It’s not something widely embraced in clinical environments, and I understand why. But still, I couldn’t ignore the pull to explore more.
This past weekend, I dove into affirmation and mindfulness videos specifically designed for pain management. What I’ve learned so far is both surprising and empowering:
- Chronic pain is real, but our brain plays a major role in how we experience it.
- After the body has healed from an acute injury, pain can continue simply because the brain remembers it.
- The more we talk about our pain, the more we may reinforce its presence in our lives.
Many of these practitioners teach that it’s possible to retrain the brain and calm the nervous system, shifting us out of the fight-or-flight response and into a space of healing. They also emphasize that this reprogramming takes time, consistency, and patience.
I’m still at the beginning of this journey, and I’m not abandoning traditional medicine. I respect it. I rely on it. But I’m also giving myself permission to explore something more.
Because after so long of not feeling whole, I believe that healing might come from a place that integrates both science and spirit—both medicine and mindfulness.
Have you ever felt the same? That maybe there’s more out there than pills, injections, and surgeries?
I’d love to hear your thoughts.
I’ve included some information from searching on Google regarding our Brain and Pain.
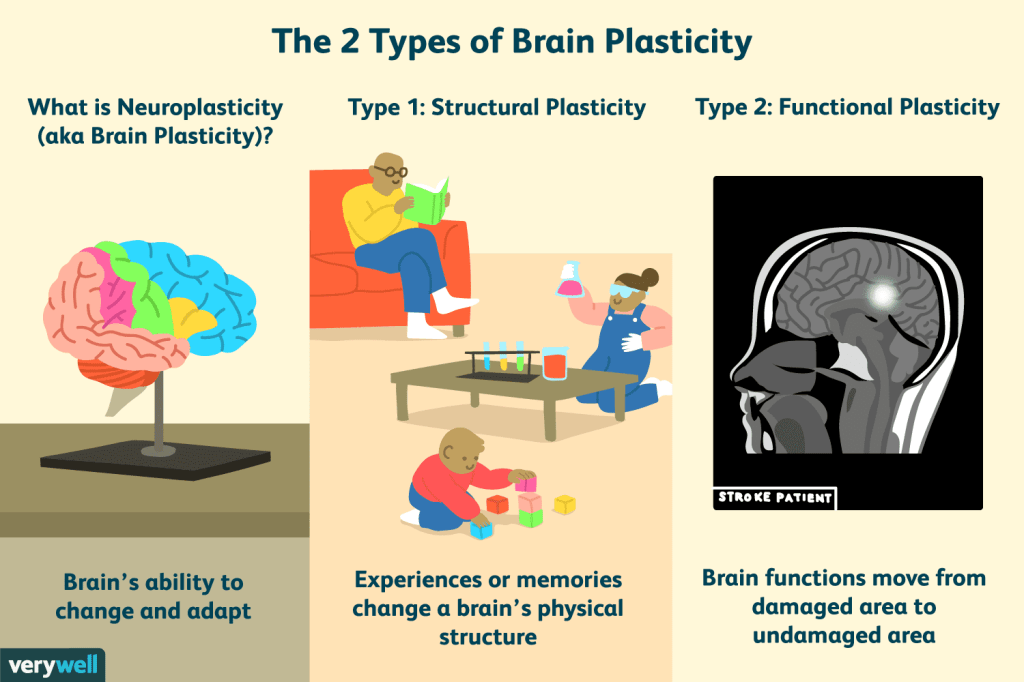
Neuroplasticity, also known as brain plasticity, refers to the brain’s ability to change and adapt by reorganizing its structure, functions, or connections throughout life, in response to learning, experience, or injury.
Here’s a more detailed explanation:
- Definition:Neuroplasticity is the brain’s capacity to modify itself, both structurally and functionally, in response to various stimuli, including learning, experience, and even injury.
- Lifelong Process:While often associated with childhood development, neuroplasticity is a lifelong process, meaning the brain continues to change and adapt throughout an individual’s life.
- Adaptation and Recovery:Neuroplasticity plays a crucial role in adaptation to new situations, learning new skills, and even in recovering from brain injuries or damage
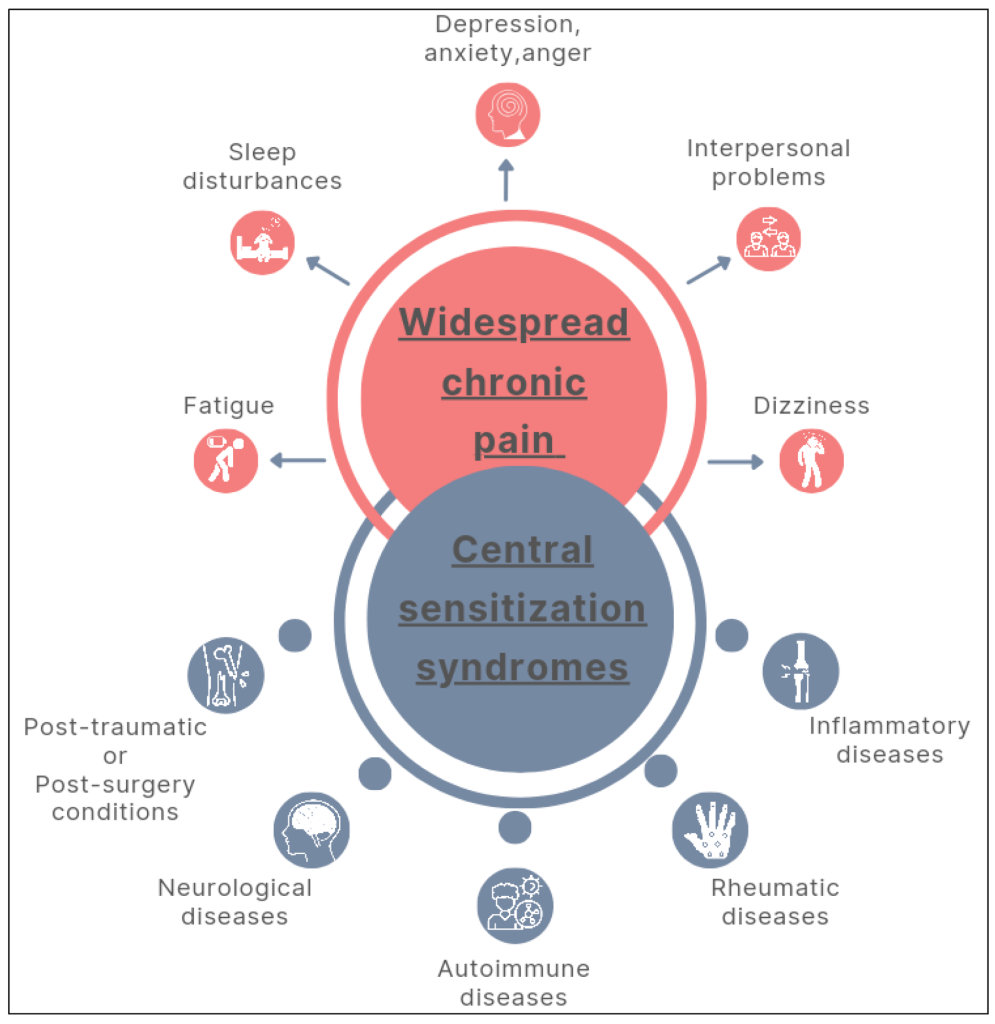
Central sensitivity syndrome (CSS) is characterized by a variety of symptoms that can include widespread pain, fatigue, sleep problems, and cognitive difficulties, often accompanied by heightened sensitivity to various stimuli like touch, sound, and light. These symptoms can be chronic, with varying intensity and duration.
LadyFlava of LadyFlavaNews
Sharing My Thoughts | Heath & Wellness


